Genetic Code vs. Zip Code – The Social Determinants of Health
“The future is already here. It’s just not evenly distributed.”
-William Gibson, Futurist
With today’s growing array of AI capabilities and the explosive growth in both the types and quantity of data available to help monitor and manage health, here’s a question: Which is a better predictor of health status – your genetic code or your zip code?
Where you live affects how you live. It impacts whether you have access to healthy food, places to exercise, or health services when needed. Your “living location” also affects your personal and family’s economic prosperity based on the availability of jobs, unemployment rates, educational and training opportunities. These “social” factors shape and determine health and longevity across your lifespan.
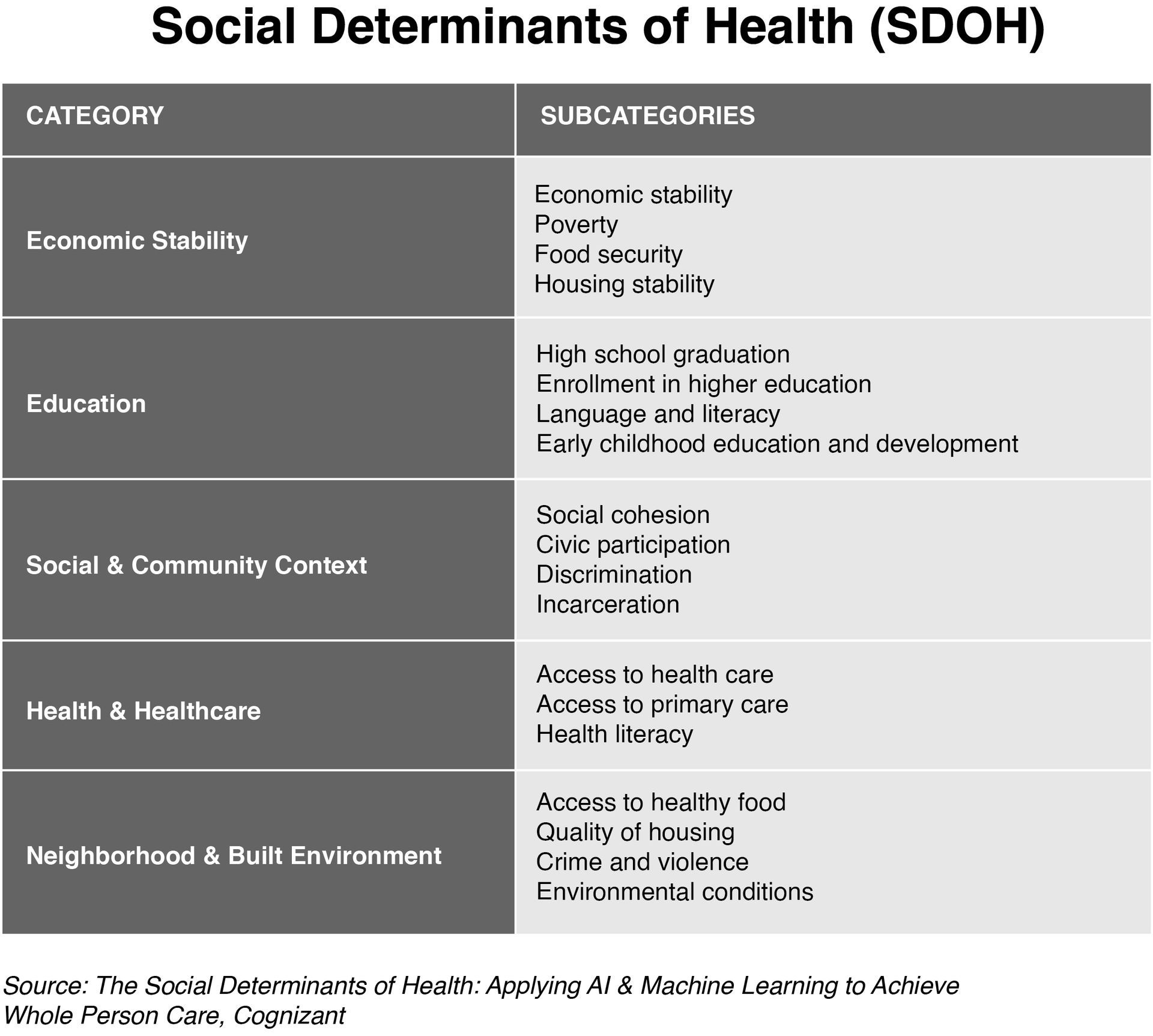
Social determinants of health (SDOH) matter when it comes to addressing how we improve the health status of individuals, communities, and nations. SDOH are conditions where people live, learn, and work that affect a wide range of health and quality-of life-risks.[i] Whether at the international, regional, state or local levels, the distribution of money, power, and resources shapes these circumstances. [ii]
Here’s an example: Two 60-year-old women live 10 miles apart in the Washington, DC area. They’ve both been prescribed beta-blockers for high blood pressure, have family histories of Type 2 diabetes, and have missed their last few annual check-ups. Shouldn’t their care plans be the same?
Clinically, they’re identical images. However, one piece of data dramatically tilts the equation. Their zip code. One will likely live 33 years longer based on their location. This dramatic life expectancy gap can be chalked up to differences in income, education, and access to grocery stores.[iii]
Traditional Health Systems have historically used data to understand the physiologic aspects of a health or medical condition. Such data is important in making diagnoses and managing health, but only shows part of the picture. Social and environmental factors are much more indicative of a patient’s health outcome than once thought. One study suggests that 60% of a patient’s healthcare outcome is driven by their behavior and social and economic factors, 10% by their clinical care, and 30% by their genetics.[iv]
Unfortunately, a study by American Health Information Management Association (AHIMA) found that while nearly eight in 10 U.S. healthcare organizations collect social determinants of health (SDOH) data many are not making good use of it because of challenges related to the collection, coding, and use of this clinically relevant data.[v]
The Color of COVID
Neighborhoods with large populations of Black Americans tend to have lower life expectancies than white, Hispanic, or Asian communities. Such racial differences reflect the places where people live, not the individual characteristics of people themselves.[vi]
The early stages of the COVID-19 pandemic gave voice to these issues. At the beginning of the pandemic, the data showed that Black Americans were twice as likely to die from COVID-19 even though they were a smaller percentage of the overall population.
In taking a closer look, two things became self-evident—first, higher death rates related to where people lived. Second, the “twice as likely to die” was a statistical average. Underneath this average was the true story. In reality, if you were Black and living in Washington DC, you were six times more likely to die of COVID at that time. Living in Michigan meant that you were four times more likely to die of COVID.[vii]
Black communities are less likely to have access to resources that promote health, like grocery stores with fresh foods, places to exercise, and quality healthcare facilities. This is true even in middle-class neighborhoods.[viii]
[ix]
[x]
Artificial Intelligence (AI) as a Turning Point
AI gives us the ability to better understand and proactively address social determinants impacting health.
To factor SDOH into health planning, health organizations must first be able to identify consumers facing adverse SDOH. Once identified, such factors can be incorporated into personal health management and population health strategies.
AI can help automate the identification of people whose health is likely impacted by their living situation. Opportunities include adding intelligent features to EMRs and proactive assessments of patient populations. Such activities help to identify and triage at-risk populations and enable organizations to build intelligent workflows for referrals and follow-up.
One study found that AI accurately predicted inpatient and emergency department utilization using only publicly available SDOH data such as gender, age, race, and address.[xi]
AI promises to make it more practical to incorporate SDOH into care management and population health strategies. AI can identify consumers whose health issues are related to SDOH and then help clinicians with targeted interventions to help them better manage their health while maximizing the use of resources.
Understanding and incorporating Social Determinants of Health in health planning is at the heart of moving toward healthier citizens and communities. We are seeing a trickle rather than a stampede of activity to leverage the power of SDOH. What can we do to make this go faster?
For a deeper dive download this
free whitepaper from the American Health Information Management Association (AHIMA).
Endnotes:
[i] Centers for Disease Control (CDC). https://www.cdc.gov/socialdeterminants/index.htm
[ii] Outright International at the UN. [ Feb; 2022 ]. 2018. https://outrightinternational.org/content/world-health-organizations-says-being-trans-not-mental-disorder
[iii] Greg Kefer, Zip codes have become a better predictor of health outcomes than genetic codes. Technology may be ready to fix that.Medcity News, August 24, 2021, https://medcitynews.com/2021/08/zip-codes-have-become-a-better-predictor-of-health-outcomes-than-genetic-codes-technology-may-be-ready-to-fix-that
[iv] Shroeder, SA. (2007), “We Can Do Better – Improving the Health of the American People,” NEJM, 357:1221-8
[v] AHIMA White Paper Identifies Opportunities and Challenges with Collecting, Integrating, and Using Social Determinants of Health Data, American Health Information Management Association (AHIMA), February, 2023, https://www.ahima.org/news-publications/press-room-press-releases/2023-press-releases/ahima-white-paper-identifies-opportunities-and-challenges-with-collecting-integrating-and-using-social-determinants-of-health-data/
[vi] U.S. Small-area Life Expectancy Estimates Project: Methodology and Results Summary, NATIONAL CENTER FOR HEALTH STATISTICS, September 2018. https://www.cdc.gov/nchs/data/series/sr_02/sr02_181.pdf
[vii] APM Research Lab. The Color of Coronavirus: COVID-19 deaths by race and ethnicity in the
U.S. Data updated as of June 10, 2020. Accessible via: https://www.apmresearchlab.org/covid/deaths-by-race
[viii] Ibid
[ix] Nicole I. Larson, PhD, MPH, RD Mary T. Story, PhD, RDMelissa C. Nelson, PhD, RD. Neighborhood Environments Disparities in Access to Healthy Foods in the U.S., American Journal of Preventive Medicine. November 03, 2008, :https://doi.org/10.1016/j.amepre.2008.09.025
[x] Rayshawn, Ray, An Intersectional Analysis to Explaining a Lack of Physical Activity Among Middle Class Black Women
Wiley Online Library, September 2014, https://doi.org/10.1111/soc4.12172
[xi] Soy Chen, MS, Danielle Bergman, BSN, RN, Kelly Miller, DNP, MPH, APRN, FNP-BC, Allison Kavanagh, MS, John Frownfelter, MD, MSIS, John Showalter, MD, Using Applied Machine Learning to Predict Healthcare Utilization Based on Socioeconomic Determinants of Care. The American Journal of Managed Care, January 2020, Volume 26, Issue 01. https://www.ajmc.com/view/using-applied-machine-learning-to-predict-healthcare-utilization-based-on-socioeconomic-determinants-of-care