Tom Lawry • November 18, 2025
Hidden Data Errors Delay Healthcare for Millions of Americans
Network inaccuracy isn’t an inconvenience — it’s a public health crisis.
Four out of five provider directory listings in major health plans are wrong.
That bad data drives higher costs, delayed care, and fear for millions of Americans already worried about getting sick.
This isn’t a complex problem to fix.
It’s a neglected one.
This article is worth reading.
T.

There’s a quiet but consequential misunderstanding happening in healthcare right now. Across boardrooms and conference stages, leaders talk about artificial intelligence as if it’s the disruption to manage—the next great differentiator between healthcare organizations. Strategies are framed around AI adoption, governance, and maturity, as though intelligence itself is the “holy grail.” It isn’t. The real disruption didn’t arrive as a technology roadmap or a vendor demo. It walked through the front door, pulled out a phone, and sighed in frustration. Your competition isn’t the health system across town. It’s the experience someone had with Amazon the night before. Healthcare is no longer evaluated against healthcare. It’s evaluated against the rest of a person’s life—and in 2026 that life is increasingly intelligent, mobile, personalized, and relentlessly convenient. That is the shift many healthcare organizations still haven’t fully internalized. Welcome to the era of the Intelligent Health Consumer. I first wrote about the rise of the Intelligent Health Consumer in my 2020 book, AI in Healthcare – The Rise of Intelligent Health Systems. At the time, the idea felt forward-looking. Today, it’s no longer a prediction. It’s simply reality. Consumers don’t wake up thinking about AI. They wake up inside it. Intelligence has become the background hum of daily life—so embedded that it’s almost invisible. A wearable quietly interprets sleep patterns and physiological signals overnight. A bank resolves fraud before anxiety ever has a chance to surface. A travel app predicts price changes with uncanny timing. A streaming service understands mood and preference like a close friend. None of this feels magical anymore. It feels normal. And that distinction matters. Because consumers don’t care how these systems work. They care about how they feel. These experiences remove effort. They anticipate needs. They deliver clarity without demanding attention. They respect time. This is the world people now inhabit—one where intelligence fades into the background and life simply works. And then a consumer enters healthcare. Suddenly, everything slows down. Tasks that should take minutes stretch into days. Answers that should be clear are buried inside portals filled with PDFs, unexplained terminology, and fragmented information. Scheduling feels transactional. Billing feels adversarial. Navigation feels like guesswork rather than guidance. Not because clinicians lack compassion or capability—but because the experience surrounding the extraordinary skills, talents, and hopes of doctors, nurses, and care teams has not kept pace with the intelligence shaping the rest of a consumer’s life. This is where the real gap lives. It’s tempting to say healthcare is falling behind. That framing misses the mark. Clinically, healthcare is advancing at an extraordinary pace. Scientific discovery, diagnostics, therapeutics, and medical expertise continue to accelerate. The problem is that everything outside healthcare is advancing even faster in how it communicates, anticipates, and personalizes. The reference point has moved. Healthcare hasn’t moved with it—yet. Consumers feel that dissonance immediately. They don’t need surveys to tell them something is wrong. They feel it in the friction, the repetition, and the lack of continuity. They feel it when every other industry seems to remember them, but healthcare still asks them to explain themselves from scratch. When that happens, healthcare isn’t compared to another hospital or health plan. It’s compared—often subconsciously—to the best experience they had yesterday. That’s why the Amazon comparison matters. Not because healthcare should behave like retail, but because consumers carry expectations forward. Seamless ordering, proactive communication, and effortless resolution become the baseline. When healthcare falls short of that baseline, it doesn’t feel “complex.” It feels outdated. At this point, many leaders retreat to a familiar refrain: healthcare is different. More regulated. More complex. More consequential. All of that is true—and also beside the point. Consumers don’t experience regulation. They experience interaction. They don’t see complexity. They feel confusion. They don’t care why something is hard. They only know that it is. Here’s the uncomfortable reality: regulation does not require opacity. Complexity does not demand friction. Clinical care may be uniquely serious, but the experience around it does not need to feel uniquely broken. The world has already reset expectations for how organizations communicate, respond, and adapt. Healthcare didn’t opt out of that reset. It simply hasn’t fully acknowledged it. What’s driving this change isn’t AI adoption curves or technology roadmaps. It’s something far more powerful: expectation inflation . For decades, healthcare transformation was driven by reimbursement changes, regulatory pressure, or policy shifts. Today, it’s driven by comparison. Consumers no longer compare hospitals to other hospitals. They compare healthcare to the best experiences they have anywhere in their lives. This is the real disruption. Not AI as a tool—but AI as a trainer of expectations. Once consumers are taught that systems can anticipate, explain, and adapt, anything that doesn’t feels outdated. Any friction feels unnecessary. Any opacity feels like indifference. The Intelligent Health Consumer isn’t waiting for healthcare to catch up. They’re already here, carrying expectations shaped elsewhere. They expect clarity without chasing it. They expect personalization without paperwork. They expect systems that remember, connect, and anticipate. They expect digital experiences that don’t require training manuals or patience. Most importantly, they don’t view healthcare as a special ecosystem with separate rules. They view it as part of life. And life, now, is intelligent. This doesn’t mean healthcare needs to become Amazon or Netflix. It doesn’t mean care should be transactional or superficial. It means healthcare must operate in a world where consumers are trained—every single day—by organizations that remove friction by default. That is the shift. The organizations that succeed over the next decade won’t be defined by the size of their campuses, the number of beds they operate, or even how much technology they deploy. They’ll be defined by how well they use intelligence to make care feel coherent, humane, and responsive. They’ll understand something essential: AI isn’t the story. The consumer is. The Intelligent Health Consumer has arrived. The only remaining question is whether healthcare is willing to meet them where they already are. T.
It was the fall of 2022 when Large Language Models and Generative AI burst out of research labs and onto Main Street. Since then, every day seems to bring another AI breakthrough that challenges how work gets done. In my role advising organizations on AI strategy and deployments, I see a consistent pattern among healthcare leaders: excitement about what AI could unlock, paired with exhaustion from the volume of noise, pressure, and competing claims. Welcome to 2026. As predictions flood inboxes and social feeds, focused on what AI might do next, I want to ground the conversation in something more useful. Rather than forecasting outcomes, let’s focus on three forces already at work—forces that will determine whether AI delivers real value in healthcare or quietly stalls. Will 2026 be a year of boom, bust, or backlash? The honest answer is yes. Boom: Early Wins—and an AI Arms Race Let’s start with what’s working. Healthcare is seeing real, if narrow, gains from AI: Ambient documentation reducing administrative burden Imaging and pathology tools improving speed and consistency Operational and revenue cycle applications driving incremental efficiency These are not moonshots. They are targeted solutions addressing specific pain points. And they matter. At the same time, healthcare is now firmly in an AI arms race. Every EHR vendor, medical device company, life sciences firm, and digital health startup is racing to declare itself “AI-native.” Roadmaps are packed with copilots, assistants, agents, and automation claims. No vendor wants to be perceived as falling behind. That pressure is accelerating innovation—but it’s also compressing timelines, encouraging over-promising, and pushing organizations to adopt faster than they can realistically absorb. Boom energy is real. But it is also uneven and fragile. Prediction: Within two years, most AI used in provider organizations will arrive embedded inside core systems and devices already in use. Intelligence will not be something teams “add on”; it will be something they inherit. Recommendation: Understand where AI is already embedded across your vendor ecosystem and what’s coming next. Engage early through advisory councils or pilots. Engage and prepare clinicians before these capabilities are introduced into workflows. AI should never arrive as a surprise. Bust: When Pilots Multiply, but Value Doesn’ t Generative AI has dominated innovation agendas, yet only a fraction of pilots ever reach sustained production. A survey cited by MIT reports that roughly 95% of business AI pilots fail to generate measurable returns. This is not evidence that AI lacks value. It is evidence that many organizations lack discipline. High failure rates are normal in early markets. Technology matures. Tools improve. But value only materializes when leaders focus on fundamentals: design, data readiness, workflow integration, and ownership. Most AI initiatives fail not because the technology doesn’t work, but because success is never clearly defined. Projects are launched out of curiosity, vendor pressure, or fear of being left behind. Clinical impact, operational accountability, and economic value are clarified too late—if at all. Equally damaging is the underestimation of the human systems AI enters. Healthcare work is relational, regulated, and trust-dependent. When AI is introduced without redesigning workflows, preparing staff, or clarifying responsibility, it creates friction—not relief. Adoption then stalls quietly. Prediction: In 2026, organizations will run fewer AI pilots—but with much higher expectations. Boards and executives will require clearer evidence of clinical, workforce, or financial value before approving new initiatives. Recommendation: Move from “fail fast” to “fail before you scale.” Define success upfront, assign ownership early, and redesign workflows alongside technology. AI initiatives without a credible path to value should stop quickly . Backlash: Fear, Workforce Anxiety, and the Trust Gap The most underestimated force shaping AI’s trajectory in 2026 isn’t technical or financial. It’s human. History offers context. When automobiles first appeared, they were seen as dangerous and socially disruptive. Red Flag laws required people to walk ahead of vehicles waving flags and capped speeds at just a few miles per hour. These laws weren’t about innovation—they were about fear, control, and adjustment. Healthcare AI is entering a similar phase. Workforce research shows healthcare workers are among the most cautious about AI adoption, citing concerns about trust, transparency, and job impact. This caution is not irrational. Healthcare has a long history of technology being imposed rather than co-designed. As a result, scrutiny is increasing—particularly from labor organizations and state legislators. Recent bills, including those limiting AI’s role in clinical decision-making and licensed practice, reflect not anti-innovation sentiment, but unresolved trust and knowledge gaps. Innovation does not scale without trust. In 2026, AI scrutiny will intensify, especially with labor organizations and at the state legislative level. As I write this, the Chair of the New York State Senate Committee on Internet and Technology just introduced a bill (S7263) to “protect patients and front-line care workers from the adverse effects of AI tools in risky or untested settings.” The bill prohibits chatbots from performing the duties of licensed nurses and puts strong guardrails around the use of AI in healthcare settings.” I often write about the need for a balanced approach to defining both the “gas and guardrails” that guide AI’s use in health and medicine. Incentives and safeguards are equally important. Prediction : Expect increased legislative activity and labor engagement around AI in healthcare throughout 2026. Such actions should not be dismissed simply as anti-innovation. They reflect something deeper: a trust and knowledge gap that needs to be closed. Recommendation: Create durable AI value by investing in workforce and consumer education. Clinicians need clarity—not just on how AI works, but on how it supports professional judgment rather than replaces it. From Awe to Analytical The year ahead will test leadership resolve. Transformation in healthcare is rarely linear—and never clean. Vendors will continue to showcase breakthroughs. The hype will continue. But 2026 is not the year for cheerleading. It is the year for realism. The most effective leaders are moving from awe to analysis—recognizing that AI value does not come from the technology itself, but from the opportunity it creates to rethink how work gets done. In that sense, AI value is—and always will be—a uniquely human process. T.
In my keynote presentations to healthcare leaders, one of the questions I always pose is this: Is AI part of your organization’s HR plan? When it comes to AI, healthcare leaders often overestimate the challenges of technology and underestimate the challenges of people. Employee resistance and lack of understanding are among the top reasons AI initiatives fail to deliver on their promise. This isn’t a criticism. It’s an acknowledgement that the single greatest question anyone in the healthcare workforce has is this: What does AI mean to me and my career? That’s why upskilling the healthcare workforce on AI basics isn’t optional—it’s mission-critical. Here are a few essentials every healthcare leader should consider when building AI fluency across their organization: ✅ Start with awareness, not algorithms. Help staff understand what AI is—and isn’t. ✅ Link learning to purpose. Tie AI education to improving care, safety, and patient outcomes. ✅ Tailor training to roles. A nurse, clinician, and administrator each need different levels of literacy. ✅ Make it continuous. AI learning shouldn’t be a one-off workshop—it’s a journey. ✅ Foster psychological safety. Encourage curiosity and open dialogue about change. ✅ Teach responsible AI. Build fluency in bias, privacy, and ethical use. AI readiness is strategic—not optional. And so, is AI part of your HR plan today? How is your organization preparing its workforce for the age of intelligent care? What steps are you taking to turn AI fear into AI fluency? T.

The Joint Commission and Coalition for Health AI (CHAI) just released the first national guidance (US) on the Responsible Use of AI in Healthcare. This is a practical, flexible framework designed to help health systems of all sizes govern, validate, and monitor AI responsibly—while ensuring patient safety and trust. Coming next: AI governance playbooks and a voluntary AI certification program for more than 22,000 accredited organizations nationwide. This is a significant step forward for provider organizations in the United States seeking a standard, well-vetted approach to responsibly deploying AI. Go here for more information. T.

I recently did the opening keynote for the annual gathering of the Forum for Healthcare Strategists to discuss the almost unlimited opportunities that forward-thinking marketing and patient experience leaders have to move us from "one-size-fits-all" to a highly personalized and effective experience for every patient and health consumer. Thank you, Chris Boyer, for interviewing me and allowing me to share my thoughts on AI and strategic marketing in healthcare. The interview may be found here . T.
I’m excited to be heading to Johannesburg in January to keynote and serve on the faculty for AMLD Africa. Love that this is an event driven by students from Africa and around the world who are dedicated to democratizing Artificial Intelligence across the continent through knowledge-sharing, ethical development, and inclusive innovation for an equitable digital future. The event is happening on the campus of Wits University January 26-29, and is geared towards students, researchers, startups, industry professionals, policymakers who are interested in shaping an intelligent future for Africa. Go here for more information: https://mlafrica.org/event/amld-africa-2026/

I was in New York last week to do the opening Keynote for the HIMSS 2025 AI Forum. It was a great international gathering to review and discuss the state of AI in health and medicine. My keynote for this event focused on how AI is driving fundamental changes in the provision of health and medical services as a backdrop to what I call the "AI Leadership Imperative." Done right, AI is not about technology. It's about EMPOWERMENT. 2025 is the year health and medical leaders must move away from Fear of Missing Out as a motive and put in place the people and processes necessary to use AI to drive value at scale across health enterprises. For a deeper look at what I covered in my HIMSS talk, GO HERE for a thoughtful review of my session by Gil Bashe of Medika Life.
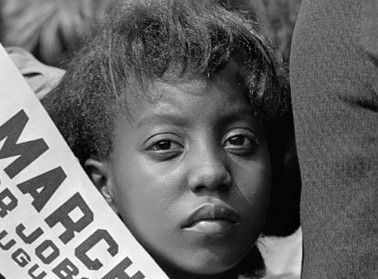
As we commemorate Juneteenth, let us recognize that, despite decades of progress, systemic disparities persist in who gets care, when, and how. These gaps are rooted in the embedded policies, norms, and practices that advantage some and disadvantage others. Health care is a noble cause, and it needs our help. I hope you will take a few minutes to reflect on the information I’ve excerpted from my new book, Health Care Nation. Each of us has the power to make a difference. Health equity isn’t just a moral imperative—it’s a path toward a more just and prosperous future for all of us. T.

This week, I hit the airwaves on Shake It Off—a talk radio show reaching listeners across the greater New York City area—to share the story behind my new book Health Care Nation. We didn’t just talk health care. We talked movement building . I believe it’s time for citizens and clinicians alike to raise their voices—not just in frustration, but in reimagining what American health care could be . If you're ready to challenge the status quo and be part of a smarter, more humane system, give this a listen .
